‘Great ease and simplicity of action’: Dr Nelson’s Inhaler and the origins of modern inhalation therapy
Abstract
https://dx.doi.org/10.15180/170807/001Unveiled at the conclusion of a meeting of the Royal Medical and Chirurgical Society in 1861,[1] ‘Dr Nelson’s Improved Inhaler’ was one of the most important milestones in the genesis of reliable treatment of respiratory ailments in the modern era. Affordable and suitable for self-medication, the Dr Nelson’s Inhaler offered simple and reliable relief for patients with respiratory and pulmonary ailments. Conspicuous for its modesty and simplicity, it was one of the most widely produced, reproduced, and used inhalation devices in the final third of the nineteenth century. By reconstructing the ‘biography’ of the Nelson Inhaler, this article will attempt to sketch a network of medical and commercial interests and expertise in London which aligned in the 1860s to help establish inhalation as a popular, inexpensive, and trusted form of medical therapy for pulmonary ailments. This article will look at what connects physicians, apothecaries, and patients in the era: the medicines and technologies that were prescribed, made, bought, and which caused wellness, side-effects, and even death. This approach allows us to develop a narrative of respiratory illness as it was experienced by practitioners and patients alike.
Keywords
Dr Nelson's Inhaler, History of inhalation therapy, history of pharmacy, history of technology
‘Great ease and simplicity of action’
https://dx.doi.org/10.15180/170807/002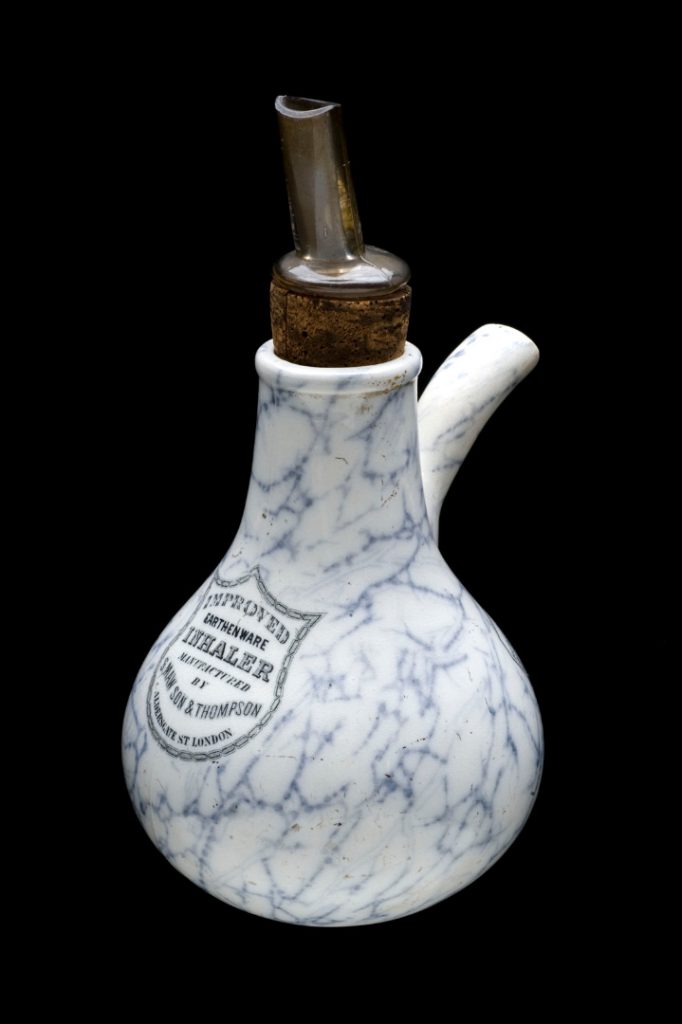
Unveiled at the conclusion of a meeting of the Royal Medical and Chirurgical Society (RMCS) – now the Royal Society of Medicine – in 1861 (Proceedings, 1861, p 399) ‘Dr Nelson’s Improved Inhaler’ was first marketed with an announcement in The Lancet in 1865 (1865a, p 152). Although mentioned only in passing in the records of the RMCS, this was one of the most important milestones in the genesis of reliable treatment of respiratory ailments in the modern era. Affordable, suitable for self-medication, requiring only steam and cheap non-prescription medication freely available from druggists and even apothecaries (British Pharmacopoeia, 1867, pp 363–364), the Dr Nelson Inhaler offered simple and reliable relief for patients with respiratory conditions. Conspicuous for its modesty and simplicity, the Dr Nelson Inhaler was one of the most widely produced, reproduced, and used inhalation devices of the period, a fact which is underlined by the sheer number and different styles of the inhaler present in the Wellcome Medical Collection housed in the Science Museum. Indeed, it is fair to describe the Nelson Inhaler as part of one of the ‘unloved collections’ in Blythe House: it is only one of a vast selection of inhalation devices that have not been regarded as suitable for display because of their technical focus or lack of aesthetic appeal. While steam inhalers were replaced in conventional respiratory medicine by modern inhalation devices (nebulizers, metered dose inhalers and dry powder inhalers) from the mid-twentieth century onwards, Dr Nelson’s Inhaler is still produced today, but it is now more usually used by voice coaches.
By reconstructing the ‘biography’ of the Nelson Inhaler, this article will attempt to sketch a network of medical and commercial interests and expertise in London which aligned in the 1860s to help establish inhalation as a popular, inexpensive and trusted form of medical therapy for respiratory and pulmonary ailments. By looking at what connects physicians, apothecaries, and patients – the medicines and technologies that were prescribed, made, bought, and which caused wellness, side-effects, and even death – we can develop a narrative of illness as it was experienced by practitioners and patients alike. Pharmaceutical therapies – medicinal products procured from physicians, apothecaries, or commercial sources such as druggists – were the most common form of medical care among the working and middle-classes over the last three hundred years or so and any history of medicine using material objects needs to begin with these cures. Lung disease was a key issue in nineteenth-century discourse and here the smallest objects and seemingly simple technologies (pills, medicated steam, inhalation devices) enable powerful and provocative accounts of both the private and socio-historical dimensions of medicine. Through its widespread availability the Dr Nelson Inhaler allows us to develop multiple narratives of medical history and its omnipresence speaks to the question of self-medication and health consumerism in the nineteenth century. Its emergence from the orbit of the RMCS, on the other hand, can also help us to reconstruct a surprisingly thorough framework of what was, essentially, quality control, which was highly unusual for pharmaceutical technologies in the nineteenth century.
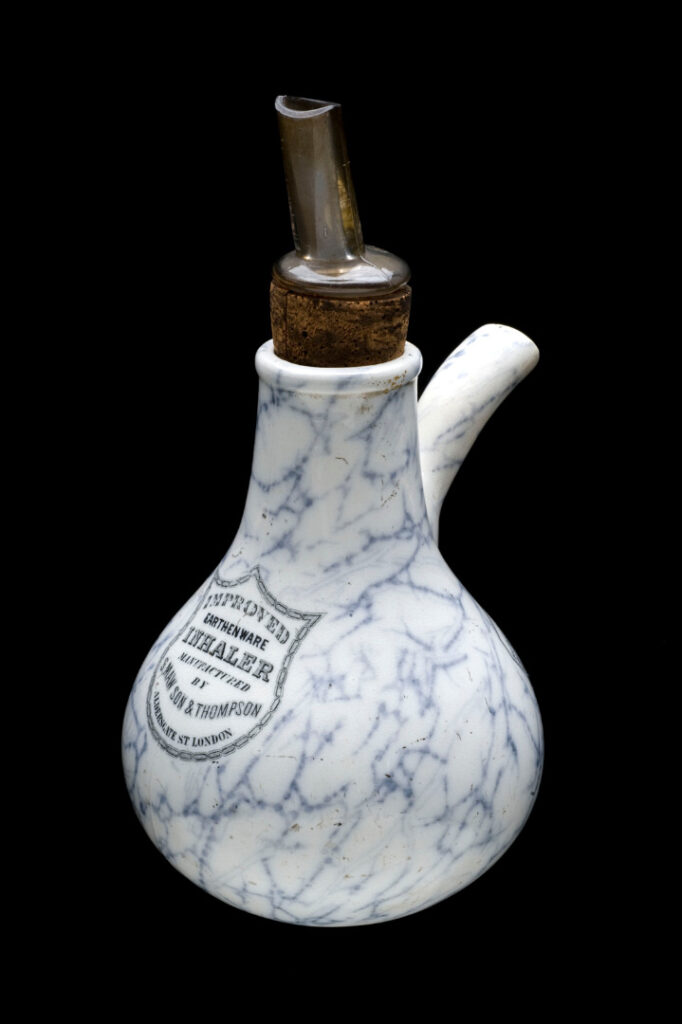
As was occasionally the practice at the regular meetings of the RMCS, a certain Dr Nelson presented his prototype for a new therapeutic device which he had designed and developed himself, at the close of business on 28 May 1861. Unlike the in-depth research papers which were read out and discussed at the meetings (and later published in the Society’s Proceedings and Transactions, including papers submitted by some of Europe’s leading medical luminaries like Edward Jenner and Rudolf Virchow), such presentations of practical devices were recorded in short, perfunctory style and without much discussion. Dr Nelson presented an inhaler, ‘its claims to notice being, great ease and simplicity of action; perfect cleanliness; and an arrangement of the mouthpiece by which is secured economy in the use of any medicated ingredient that may be required for inhalation’ (Proceedings, 1861, p 399). The inhaler consisted of a small ceramic ‘pot’ with two protruding openings. The opening at the top of the device could be blocked with a cork into which a short metal tube was inserted to form a mouthpiece (in later versions glass was sometimes used); another spout-like outlet to the front remained open. According to directions in The Lancet, hot water was to be poured into the main body of the inhaler while the medication was to be soaked on a sponge inserted below the corked opening at the top. The patient would inhale through the mouthpiece, drawing in air from the second opening through the water and steam. This would potentially vaporise the medication on the sponge and deliver it to the lung.[2]
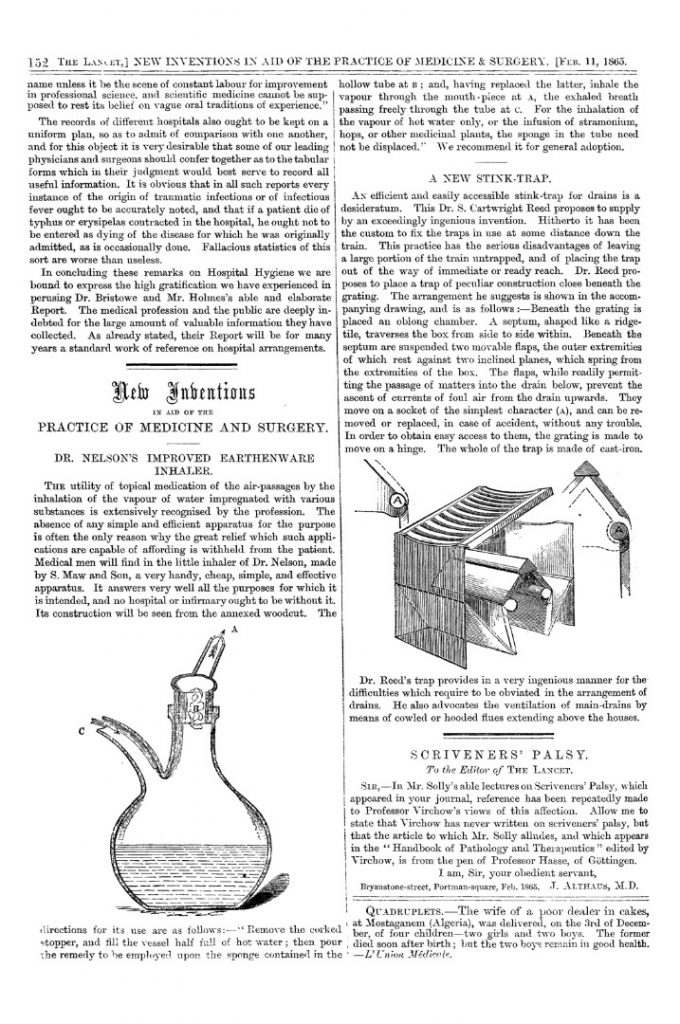
By 1865 Dr Nelson’s device was being advertised widely in journals such as The Lancet (1865a, p 152), The Medical Times and Gazette (1865b, p 160) and later in the British Medical Journal (1870, p 674). Now christened ‘Dr Nelson’s Inhaler’, this new inhalation device was produced and marketed by S. Maw & Son from their London base in Aldersgate Street near the present-day Barbican (Maw’s, 1866, p 82; Maw’s, 1870, p 66). Maw’s was a well-established surgical instrument provider, but they also sold less specialist medical products for the domestic market such as plasters, syringes and bandages. Following in the footsteps of pioneers like Mudge and Ramadge, the company had already begun advertising various inhalers in the early 1840s and later sold devices such as ‘Startin’s Pneumatic Inhaler’ for the new chloroform and ether anaesthesia, making the company an ideal partner for inventors of new respiratory devices (Illustrated Catalogue, 2014, Vol. 2, p 125).

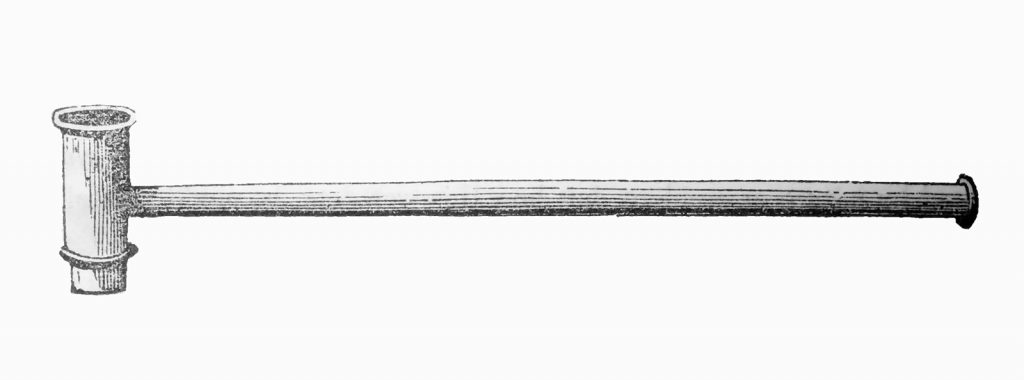
Dr Nelson’s Inhaler did not emerge into a vacuum in the mid-nineteenth century. John Mudge had invented a pewter inhaler in 1778 and seems to have been the first physician to use the word ‘inhaler’ in his related case histories (Mudge, 1778, p xi). Nelson’s most immediate predecessor was Francis Ramadge, however. Ramadge developed an inhaler for treating tuberculosis and asthma which he made more widely known through his publication Consumption Curable in 1834 (Ramadge, 1834, pp 85–87). Born in Dublin and educated in Dublin and Oxford, Ramadge was senior physician and lecturer at the Central Infirmary in London, where he specialised in respiratory diseases. His inhaling pipe was a narrow tube made of wood or ivory through which the patient inhaled and exhaled. Initially it was about four feet long, but later designs were much shorter and included a whistle-type valve (Fitch, Six Lectures, pp 93–95). The narrow tube provided resistance to inspiration and expiration, and the therapy was designed primarily as a palliative ‘mechanical’ exercise to strengthen the lungs and expand the chest (Ramadge, 1834, p v). Interestingly, technologies are still employed today for respiratory muscle training in chronic obstructive pulmonary disease and cystic fibrosis using inspriatory/expiratory resistance devices (Volska et al, 2003; Battaglia et al, 2009; van Winden et al, 1998). While he acknowledged his indebtedness to experiments with inhalation by René Laennec (Ramadge, 1850, pp 9–12) and by Beddoes in Bristol (Ramadge, 1835, pp 109–110), Ramadge was sceptical about the efficacy of inhaling medical preparations: ‘As to medicated vapours […] upon the whole, I have found them to be either useless or injurious’ (Ramadge, 1850, p 10; see also Ramadge, 1834, p 91). Notwithstanding these misgivings on inhaling medicinals, the version of the device advertised by Maw & Sons in the 1860s shows Ramadge’s pipe leading from a Mudge-type tin which would have been filled with hot water infused with pharmaceutical preparations similar to those used in conjunction with the Nelson’s Inhaler (Maw, 1866, p 81). This would suggest that by the mid-nineteenth century both the mechanical and pharmaceutical uses of inhalation had become linked, even if Ramadge himself may have had little say in the design anymore (he died in 1867).
These technical innovations in inhalation therapy were not confined to Britain. In continental Europe considerable progress was being made in developing nebulizers, a more complex technology than the simple steam inhaler favoured by Mudge, Ramadge, and Nelson. In 1849 Auphon invented his ‘atomizer’ in Euzet-le-Bains, the point of origin of all further nebulising devices in the nineteenth century. His invention involved shooting a jet of medicated water at a metal plate, the resulting spray being inhaled by the patient. The models for this device were the inhalation rooms at spa resorts, where water would be jetted at the heated walls of an inhaling room, the pressure and heat producing a spray which was inhaled by walking around the room. In 1858 Jean Sales-Girons, well-known as the editor of the respected journal La revue médicale, introduced a portable version of this nebulising effect, using a small pump operated by the patient himself to generate the pressure required to produce the spray of medicated water which would be inhaled through a funnel-like mouthpiece (Sales-Girons, 1861, p 10). A similar device was developed and marketed by James Dewar in Scotland in the mid-1860s (Dewar, 1868, p 48). Dewar recommended a system of ‘disinfecting’ the nose, throat, and lungs with sulphuric acid (p 9). In Germany, in 1862, the Berlin lung specialist Louis Waldenburg acquired one of Sales-Girons’ devices and adapted it with a design familiar from perfume sprays. He replaced the complicated and irregular pump in Sale-Girons’ device with Mayer’s uterus douche, which was to be operated by hand (Anon, 1862, p 330). In the same year in Berlin J Bergson, Georg Lewin’s successor in the Inhalatorium at Berlin University, advertised his ‘Hydrokonion’ nebulizer on which he had been experimenting for some years (Bergson, 1862, p 389). His design replaced the hand-pump of previous nebulizers with two small tubes at right angles to each other, using a small foot-pump and the Bernoulli pressure principle to draw water up through one pipe and generate a spray with the other (Bergson, 1863, pp 66–67). In Stuttgart Emil Siegle developed a widely respected steam spray inhaler which used heat to generate the steam necessary for the Bernoulli principle, thereby rendering the hand-pump redundant (Siegle, 1864). His device consisted of a glass bulb filled with water from which one tube emerged to disperse the steam generated from by a small paraffin lamp at the base of the device. The medication was carried through a short tube from a second glass receptacle and was nebulised by the steam. The patient inhaled the medicinal steam through a small glass funnel (Siegle, 1864, p 25). Siegle’s apparatus was manufactured and distributed in Britain by Krohne and Sesemann from 1871 onwards (Grossmann, 1994, pp 55–64; Anderson, 2005, pp 1139–1150; Sanders, 2007, pp 71–81) and although under patent (‘Announcement’, 1864), it was quickly adapted by British physicians such as James Maxwell Adams in Glasgow (Adams, 1878). Siegle’s patent officer in London, George Davies, clearly objected to the infringement and stopped Adams from marketing his inhalation device. Siegle for his part seems to have copied Adams’ major innovations to improve his own device, adapting the boiler and replacing the glass components with more sturdy metal receptacles and face-guards (Adams, 1878, p 3). Owing to its Europe-wide success, Siegle’s inhaler is generally held to be the first nebulizer in the proper sense.
While the Dr Nelson’s Inhaler appears somewhat old-fashioned by comparison with these nebulizers, it was in fact revolutionary at the time for its ease of use and patient-friendliness. It predated the availability of the Sales-Girons-type and Siegle-type nebulizers in Britain by some five years, and even after these other devices were available, the Nelson’s Inhaler required a fraction of the maintenance necessary for the small technical parts in the nebulizers. Unlike these other devices, Dr Nelson’s invention contained no complex tubing mechanisms to keep in working order and no sensitive components like glass which were prone to breaking and needed replacement. These factors made Nelson’s Inhaler significantly cheaper. It was available for a relatively low price of between 4s and 5s 6d. By contrast the Ramadge Inhaler cost 16s (and required additional purchases of tubes, starting from 3s each), Mudge’s Inhaler started at 8s (Maw Son & Thompson, 1866, pp 81–2), and when the Siegle Inhaler emerged on the market in the 1870s it was sold by Krohne & Sesemann for between 7s 6d and £3 5s (Krohne, 1878, p 102).[3] The replacement parts for these nebulizers were pricey, costing between 1s 6d and 3s. In terms of cost and ease of purchase, Dr Nelson’s Inhaler was significantly more customer-friendly. That said, given that average weekly earnings of labourers and artisans was 20s–30s in 1860s London, even the Dr Nelson’s Inhaler would have been an exorbitant investment for the working classes. This suggests that the main consumer group for the inhaler were the aristocracy and the growing classes of professionals, clerks, civil servants, and army officers, who earned in the region of £4–£5 a week, or £200–£300 annually (Porter, 1998, p 176).
The question of accessibility is no less important than affordability. Both Dewar’s version of the Sales-Girons inhaler and Siegle’s inhaler were initially only available for purchase from the instrument makers themselves (in Kirkcaldy and London respectively). From the outset the Dr Nelson’s Inhaler could be purchased directly through pharmacies or by order from Maw & Sons for use at home. This ease of access also had therapeutic reasons: Sales-Girons, Bergson, and Siegle all recommended using their devices under instruction in their clinics and inhalatoria, whereas the Nelson’s Inhaler could be used under the instruction of a physician (e.g. in private practices or in hospitals) or procured for private use at home. This was in part because of safety aspects involved: early versions of the Siegle Inhaler were criticised for their dangerous unreliability. According to James Adams, the glass boiler was fragile and was prone to overflowing, potentially scalding the patient: ‘the water flowing over through the stream escape is projected forcibly in the face of the patient’ (1878, p 10). In Adam’s opinion ‘it required much persuasion on the part of the physician, and considerable nerve on the part of the patient, to face Siegle’s Patent Inhaler after one or two experiences of this nature’ (ibid). While steam inhalers such as Dr Nelson’s device and nebulizers such as those patented by Siegle and Adams both used the same basic method (i.e. steam) to transport medicinal preparations, there was little danger of accidental scalding of this nature with the simple ceramic jug.

Alongside cost and maintenance, the Dr Nelson’s Inhaler required very little assembly; in fact, it could be used exactly as purchased. The mouthpiece remained attached to the cork, which would be removed to pour in hot water, and other than soaking the sponge with the medicinal preparation the patient needed to do very little to gain relief. There were also virtually no maintenance issues, other than occasionally replacing the sponge (any sponge would do) and washing out the ceramic pot. This may have been one reason why the Dr Nelson’s Inhaler was popular among patients and practitioners. The medical substances for inhalation needed to be procured separately, and these included (according to the British Pharmacopoeia of 1867) hydrocyanic acid, chlorine, tincture of iodine, creosote, and hemlock. Other common preparations suggested in advertisements but not listed in the Pharmacopoeia included henbane, vinegar, and tincture of benzoin (e.g. Friar’s Balsam), all of which were widely available as over-the-counter preparations from apothecaries, druggists, and other unofficial retails units.
Literature, case histories, and personal accounts give little indication of how long each period of use would have lasted. However, Horace Dobell recommends that the water should not exceed 170 degrees when inhalation begins (Dobell, 1872, p 203), and William Abbotts Smith generally recommends three vapour inhalations per day, with each session lasting between 15 and 20 minutes (1869, pp 60–61, p 72). Other inhalers include detailed instructions according to which patients were initially recommended to undertake one daily session of five minutes’ duration, rising to as many as ten daily sessions lasting up to fifteen minutes as the patient grew accustomed to the therapy (see Siegle, 1865, p 30). Repetitions of this duration will not have required much replenishment of hot water during each individual sitting with the Dr Nelson’s Inhaler.
Little is known about Dr Nelson and there may have been many professional reasons for this anonymity. One reason may have been the link in the public mind between inhalation therapy and quackery following a trial involving Dr Hunter (who claimed to have healed consumption through the inhalation of oxygen) and the Pall Mall Gazette in 1865–66 (Parry, 2000, pp 108–109). This could well have made a respected physician reluctant to be identified with an inhaler he had invented regardless of how successful or effective it was held to be by his peers. There was clearly potential for reputational damage that could be incurred by having one’s name associated in advertisements for inhalation devices or remedies, with the whiff of so-called quackery literally in the air. For example, in the first edition of his On Affections of the Throat and Lungs, Abbotts Smith included a preface distancing himself from Hunter’s ‘ignorant’ and ‘reckless’ treatments (Abbotts Smith, 1869, p 6). Although quack medicine, as an outgrowth of the general industrialisation and commercialisation of medicine in the eighteenth and nineteenth centuries, was by no means the sole terrain of unqualified tradesmen (qualified physicians and apothecaries also engaged in commercial activities and the BMJ was an important site for advertising), professional physicians often based their superior status on the moral integrity of not advertising (Porter, 2000; Bartrip, 1995, pp 191–204). Given the professional medico-scientific forum of the RMCS in which Nelson’s inhaler was first presented, we can assume that the inventor’s anonymity was in accordance with an unwritten code of ethics which held that the inventions of scientific and medical research should be made available for the benefit of the widest public possible (Gabriel, 2014).
While the patent records for the nineteenth century in Britain are far from complete, it is telling that there appears to have been no patent taken out on the Dr Nelson’s Inhaler and indeed the speed with which other producers advertised their own identical versions of the design (including, most notably, Boots towards the end of the nineteenth century) are evidence that there was no patent granted. The physician’s interest in the greatest medical good over egocentric profit may well have been one reason for his passing over the design to Maw & Sons to produce and market. Nevertheless, circumstantial evidence allows the possible inventors of Dr Nelson’s Inhaler to be narrowed down to two candidates. Using the Medical Register, which was first published in 1859 and included the names, addresses, and qualifications of all licensed medical practitioners in the UK, 11 individuals with the surname ‘Nelson’ who were qualified prior to 1860 can be identified, of which two – David Hume Nelson of Birmingham (ca. 1812–1901, qualified 1848 in Edinburgh) and Thomas Andrew Nelson of London (ca. 1812–1894, qualified 1834 in Edinburgh) – are the most probable candidates.
David Hume Nelson led a colourful and notable life. Born in Edinburgh, he moved to London around 1835, spent some time in prison for theft, returned to Edinburgh to qualify for his MD in 1848, before being elected physician at the Queen’s Hospital in 1849 and joining the Faculty at The Queen’s College in Birmingham shortly afterwards (Sanders and Harper, 2014). David Hume Nelson’s qualifications in respiratory medicine are also well founded, having published his dissertation On the principles of health and disease in 1850 and featured in a series of case histories in the Provincial Medical and Surgical Journal (PMSJ, a forerunner to the BMJ) around 1850–1851 (Anon, 1850a; Anon, 1850b; Anon, 1851). As part of a ‘strictly introductory’ (Anon, 1850c, p 41) series of clinical lectures serialised in the PMSJ between 1851 and 1853 (also published in book form in 1850), David Nelson also gave three lectures on ‘The morbid condition of the lungs and respiratory tubes’ (Nelson, 1851, 1853a and 1853b). It is notable that inhalation is not mentioned as a form of treatment in any of these lectures, focusing instead on more traditional ‘heroic’ humoral cures such as blood-letting, cupping, leeches and the use of mercury, antimony, and oral expectorants. Following these early publications, David Hume Nelson seems to have turned his attention to other clinical matters, publishing a series of articles in the British Medical Journal between 1860 and 1863 on ‘ferro-albuminous’ treatments and peptic acids, all of which resulted from a ten-year clinical study in Birmingham into Bright’s disease concluding in 1860 (Nelson, 1860a; Nelson 1860b).
While David Hume Nelson was a renowned physician and indeed published results from his research – albeit on a completely unrelated topic to inhalation – in the issue of the BMJ immediately following the record of the RMCS meeting that mentions the presentation of the inhaler (Nelson, 1861, p 645), Thomas Andrew Nelson is virtually unknown. It is known that Thomas Andrew qualified in Edinburgh with a dissertation on ‘Phthisis pulmonaris’ in 1834 (and thus had specialised in a related topic; see Edinburgh Journal, 1834, p 490). He then relocated to London where he lived and worked in the area around Regent’s Park, at first in Wimpole Street, then in Nottingham Terrace off York Gate.[4] Although he published few or possibly no writings whatsoever, Thomas Andrew Nelson was the only Nelson who held a Fellowship at the RMCS in the period in question, and his residence in an exclusive part of Marylebone is evidence that although we know little about him, his practice clearly thrived over a considerable period of time in the geographical area favoured by the Harley Street establishment.[5] Indeed, it is notable that highly respected physicians and experts in respiratory diseases and their treatment like Sir Charles Scudamore also lived in Wimpole Street and around York Gate in the period immediately following Thomas Nelson’s relocation to London around 1835, suggesting a community of like-minded inhalation specialists within the RMCS and in close geographical proximity (the list of members includes addresses for Nelson, Scudamore, and other establishment physicians). The Proceedings make it difficult to establish the identity of the inventor with complete certainty: a Dr Nelson only appears twice in the minutes of the meetings in this period. Unlike external speakers or guests who are listed with their full names, titles, and affiliations, however, Dr Nelson is recorded without his first name, upholding the usual practice when referring to members of the Society. As Thomas Andrew was the only Nelson in the RMCS at this time, this could at least indicate his intellectual ownership. Thomas Andrew seems to have retired in 1890 or 1891 because his name disappears from the list of members several years before his death is recorded in the Marylebone parish records for the year 1894.[6]
Although the inventor’s identity remains somewhat uncertain, Dr Nelson’s decision to work with Maw & Sons is easier to reconstruct and understand. Not only was the company at the forefront of manufacturing and supplying medical equipment to hospitals and medical practitioners in Victorian Britain, they had themselves already marketed older ceramic inhalation devices and displayed these at the 1862 Exhibition. In 1835 Solomon Maw had taken over the company, originally founded by his father George Maw in 1814, from his elder brother John Hornby, and following Solomon’s death in 1861 his son Charles ran the business in partnership with John Thompson (Anon, 1917, p 42). Maw & Sons were particularly well suited to making ceramic instruments as one of George’s sons, John Hornby Maw, had settled in Shropshire by 1850 and had set up a new business designing and manufacturing encaustic tiles, first in Worcester, then in Brosely, and finally Benthall (Herbert, 2005). With these family connections to the ceramics industry in Shropshire, and their own manufacturing and marketing expertise, S. Maw & Son were an obvious partner for the inventor.
The Dr Nelson Inhaler emerged into a medical market with a clear demand for reliable therapies for the various respiratory diseases blighting the towns and cities of industrial Europe. Rapid urban development had led not only to the spread of waterborne diseases like typhoid and cholera, but also to a peak in ailments like asthma and consumption, with fogs, smoke, and other pollutants a cause of almost constant suffering throughout the 1800s. In the Medical Times and Gazette the London Fog that killed 273 people as a result of bronchial complaints in 1873 was reported as ‘one of the most disastrous this generation has known. To persons with cardiac and respiratory disease it has in numerous instances proved fatal’ (Anon, 1873, p 697). Indeed it is telling that Maw’s – one of the largest suppliers of medical and surgical instruments in Britain – displayed various patented inhalers at the International Exhibition of 1862 (Illustrated Catalogue, 2014, p 125), a reflection of the close and difficult relationship between Victorian industrialisation and medical innovation.
Inhalation was becoming recognised as a quicker, less dangerous, less invasive, and pharmacologically more effective manner of medication for constitutionally weak consumptive patients. As indicated by the origins of inhalation therapies across Europe in spa resorts, the main forms of palliative therapy involved travelling to suitable locations such seaside baths and thermal baths, or even further afield to warmer climates (Waldenburg, 1864, p 2; Hassall, 1879), but this was unaffordable for all but the very affluent classes. More inexpensive forms of therapy included smoking stramonium and other substances, but although these provided relief, they were also known to have narcotic side-effects. Likewise, given that asthma was frequently held to be a nervous and/or spasmodic disorder, the ubiquitous opium was recommended as a relaxant in the form of pills or tinctures such as laudanum (Waldenburg, 1864, p 3; Thomson, 1866, p 37), but this was known to have significant side-effects such as constipation and addiction. Surgery was seldom considered suitable, and was concentrated on the upper respiratory tract with operations on the larynx or tonsils. Inhalation, by contrast, was growing more and more popular among physicians. In 1829, James Murray had already argued that ‘bathing the lungs’ ensured a more focused delivery, ‘local affections […] which can be directed to and confined upon any point or part affected’ is the preferred form of pharmaceutical therapy (Murray, 1829, p 168). Murray mentions Mudge’s pewter inhaler as the impetus for the renaissance of the medical procedure of inhaling vapours in the mid-1800s, but he is also critical of the practice and technology of inhalation: ‘It is needless to say that they [the inhaled vapours] do little good in the manner they are applied’ (ibid). Five years later, Charles Scudamore praises inhalation for not affecting the stomach of respiratory patients in addition to their pulmonary distress (Scudamore, 1834, pp 136–7). When Dr Nelson emerged with his new double-valve inhaler in the early 1860s it was no surprise that one of the first advertisements for the device recommended the inhaler’s simplicity (Anon, 1865b, p 160).
By the mid-1860s medical journals and other publications were full of advertisements and announcements of new types of inhalers, hence it is not surprising to find Dr Nelson’s Inhaler being advertised widely in journals such as The Lancet and the British Medical Journal in 1865. But professional colleagues like Abbotts Smith in his On Affections of the Throat and Lungs and their Treatment by the Inhalation of Gases and Medicated Vapours (1869, p 72) also recommended the device to their patients. Abbotts Smith also provides the theoretical background for the new-found popularity of inhalation therapy in the mid-nineteenth century. While stressing the impact of urbanisation and industrialisation with their economic and environmental factors, he points towards a paradigm change in drug delivery which seems to have started towards the end of the eighteenth century (Abbotts Smith, 1869, pp 16–19). While inhalations had been recommended in Egyptian, Indian, Greek and medieval treatises, most notably by Hippocrates and Maimonides,[7] Philip Stern’s marketing of his own recipe of balsamic vapours in Medical Advice to the Consumptive and Asthmatic Peoples of England of 1764 marks the beginning of a process that led to Mudge’s pewter inhaler. Stern was one of the first commercial scale producers of inhalers and inhalants and his ‘pamphlet’, which was aimed at the broader public, went through multiple editions;
the price he seems to have paid for this popular focus was that he was shunned by the medical profession of the day and his work is largely unreferenced anywhere. Experimentation with oxygen and nitrous gases by Thomas Beddoes and Humphry Davy at the Pneumatic Institute in Bristol in the 1780s and 1790s confirmed the suitability of the lungs as a site for the absorption of medicinal products. Following Beddoes’ lead, widespread experiments with oxygen and gas therapy in continental Europe, and France in particular (Lavoisier, Demarquay), showed a more widespread interest in the inhalation method around 1800. After training to administer foul-tasting medicines and invasive therapies like any other eighteenth-century physician, Beddoes noted ‘the eagerness with which these patients looked forward for their dose of air’ – the stimulus for a less invasive form of therapy was clearly motivated by these experiments (Beddoes, 1799, p 20; see also Jay, 2009; and Vickers, 2004). The publicity surrounding the Pneumatic Institute’s experiments with nitrous oxide around 1798–1800 was also the impetus to wider experimentation with chloroform and laughing gas as anaesthetics on both sides of Atlantic in the 1830s and 1840s, with the successful experiments by James Young Simpson in Edinburgh confirming the ability to generate pharmacological effects through pulmonary drug delivery.
This changing understanding of drug delivery was obviously of particular importance for physicians interested in respiratory illness. Scudamore introduced the findings of his clinical trials of inhalation in respiratory patients as follows: ‘It constitutes a new method of treatment to administer by inhalation those medicinal agents which the science of modern pharmaceutical chemistry has brought to light; and it is my object […] to show that they are capable of exerting a very important and beneficial influence in certain states of pulmonary and bronchial disease’ (Scudamore, 1830, p 2). Apart from programmatically highlighting the innovative nature of this therapy, Scudamore also points towards a changing understanding of pharmaceutical therapy to a more localised and directed form of drug delivery when he writes that the ‘rationality of applying some remedial agent in a direct manner to the seat of the disease will not be questioned’ (ibid). Similarly, Murray demands application of medicinals ‘locally to the lungs’, claiming ‘if you inhale vapour, which condenses in the cells, at least a small part of it, it bedews and covers the surfaces and ulcerations’ of the lungs, hence acting directly at the source of the irritation (Murray, 1829, p 173 and p 180). Alongside its appeal as a less physically invasive remedy, the practice of inhalation may therefore also be seen as part of a general trend towards targeted drug delivery and action emerging in mid-century Victorian Britain.
As these empirical trials show, the inhalation device was used by hospitals for the poor, but its immediate target audience will have most likely been wealthy customers who could afford to purchase the inhaler and who could thus be encouraged to self-medicate. However, the economic means to buy proprietary medicines were not limited to very wealthy patients – the type of private patients Scudamore and Thomas Nelson will have seen around Marylebone – and the ease of access to the Nelson Inhaler and related medicines like Friar’s Balsam suggest that less prosperous patients were also able to gain some relief from respiratory conditions. Such groups will have been more immediately affected by the environmental pollution of the industrial age than wealthy patients around Regent’s Park, of course, and in acute cases those patients who were too poor to be able to self-medicate will also have had access to treatment by physicians like William Abbotts Smith who worked in Finsbury Dispensary and the Metropolitan Free Hospital, both in the immediate vicinity of Maw’s base to the East of the City of London. Abbotts Smith refers to studies of patients with depositions of coal-dust in their lungs in the Sheffield area (1869, p 81) and to ‘chimney-sweeps, bakers, and dock-labourers’ (1869, pp 81–82). Indeed, he clearly drew on such patients as the clinical evidence base for his published writings, which contain various formulations which suggest that his therapeutic models are based on evidence he has gathered in the clinical environment. See, for example: ‘Several of my patients […]’ and ‘cases have come under my notice’ (Abbotts Smith, 1866, p 32); ‘The inhalation of oxygen has been found very useful in preparing delicate patients for surgical operations, by restoring their vital powers […]’ (Abbotts Smith, 1869, p 27); ‘At this stage, the effects vary according to the individual’ (ibid, p 48). In these publications, he also recommends the Nelson Inhaler unconditionally for hospitals and private patients alike:
There are numerous methods by which the patient may be enabled to inhale the steam, as, for instance, from a jug or basin containing hot water, or by breathing through a sponge which has been previously dipped in boiling water, and then partially wrung out. Several forms of apparatus have also been devised for this purpose; two of the most efficient of these, whether for the inhalation of simple steam or of medicated vapour, are Nelson’s Inhaler and Sturt’s Inhaler.
The fact that a physician recommends the Nelson Inhaler here on the basis of empirical evidence from a clinical environment is quite a surprising finding in the broader context of nineteenth-century healthcare.
Beginning with the initial presentation to the RMCS in 1861, and subsequently sanctioned in the Society’s official publication, the Proceedings, the speed with which the Dr Nelson’s Inhaler was recommended in the various media of the day is somewhat surprising. It is difficult to compare an inhaler to products such as pills, tinctures, and tonics, but these may provide a useful point of comparison. Concurrent developments in communication media, the expansion of the press landscape, and the speed of the postal network all assisted in the rise to fame and widespread use of preparations such as the laudanum brand ‘Black Drop’, tonics like ‘Lydia Pinkham’s Vegetable Compound’, and later Burrough’s and Wellcome’s ‘Tabloid’ brand of pills, with their fully-fledged advertising campaigns. In mid-Victorian Britain, advertising was still considered the domain of ‘quack’ medicines, however. In an age in which some doctors were nevertheless far from media shy (Morell Mackenzie, as an ENT specialist and inventor of the so-called ‘Eclectic Inhaler’, notoriously courted media attention, not least during his treatment of the Prussian crown prince’s throat cancer in the 1880s), the inventor of the Nelson’s Inhaler seems to have had little pretention to public renown either for his device or for himself. A comparison to the other inhalation devices mentioned in this article shows just how unusual Dr Nelson’s reticence was in this regard; Waldenburg (1862), Siegle (1864), Dewar (1868), Adams (1878), and indeed other physicians like Mackenzie, with his ‘Eclectic Inhaler’ (1880) all advertised their inventions with extensive user manuals and booklets, even if these were aimed either at professional colleagues or were distributed with the devices after they had been purchased. Dr Nelson’s reticence to use his professional respectability more visibly could have been a hindrance to the inhaler’s reception, despite his good connections in the medical community in either London or Birmingham. How should we understand the success of the device, then?
The unusually speedy success seems to have been the result of widespread acceptance among colleagues, the commercial interests of Maw & Sons, and finally the relative value for money already discussed above. For serious physicians or pharmacists, the sign of acceptance for a pharmaceutical preparation was its professional acceptance in the British Pharmacopoeia, the official sanctioned list of medication, rather than its popularity or profitability. For pharmaceutical technology the equivalent acceptance came in the form of recommendations in therapeutic handbooks, scientific studies, and its use in professional practice. This can be measured by the articles written by colleagues in specialist journals read primarily by other professionals and in more popular domestic handbooks in the final third of the nineteenth century. Readers of Spencer Thomson’s revised Dictionary of Domestic Medicine and Household surgery in 1866, for example, will have found detailed notes – including two large illustrations – on the Dr Nelson’s Inhaler (‘an apparatus for the inhalation of ether, chloroform, henbane, creosote, vinegar etc., in affections of the throat and bronchial tubes, asthma, consumption, etc.’) in the relevant article on inhalers (Thomson, 1866, p 52). In a lecture published in the BMJ and subsequently republished in various regional medical journals across Britain and North America, the eminent Professor of Materia Medica and Medicine at King’s College London, George Johnson, also spoke of having used the inhaler in advanced respiratory patients (Johnson, 1869, p 434). Finally, R Douglas Powell of the Brompton Hospital for Consumption and Diseases of the Chest, writing in The Lancet in 1877 recommends that inhalations ‘may be taken very well from a deep jug or a Nelson’s inhaler with the sponge removed’ (Powell, 1877, p 152). Colleagues were recommending Dr Nelson’s Inhaler on the basis of their experience in a clinical environment, a sign of esteem that may go some way to explaining the great success of the device in the period.
Such professional acceptance took time, however, and certainly more than the short period between 1861 (when Dr Nelson’s invention was announced) and 1865 (when it was first marketed) would have allowed. Here we must consider the role of Maw & Sons, the original producers and marketers of the device. There was indeed a relatively robust advertising and marketing campaign surrounding the Dr Nelson’s Inhaler in the 1860s and 70s across various media (from newspapers to professional journals), and this could have potentially brought the device close to accusations of commercial interests, and hence quackery. Since Dr Nelson had clearly forfeited his ownership of the device, however, these commercial interests were legitimate and didn’t impact on the medical integrity of its inventor. From the outset, the advertising also made a point of avoiding the impression of aiming at a mass audience. The first announcement in The Lancet was targeted directly at ‘medical men’ (1865a, p 152) and subsequent advertising campaigns focused on journals such as the BMJ; advertisements in more popular newspapers towards the end of the century avoided any form of excessive rhetoric. Dr Nelson’s Inhaler brought together professional dignity and acceptance, then, but also commercial know-how at an arm’s length from the medical professional himself, and finally a competitive pricing structure, making the device affordable both for public clinics or hospitals and private patients alike. The combination of commercial and professional acceptance is perhaps the most notable feature of the Dr Nelson’s Inhaler.
Unusual in that it profited immensely from both professional and commercial networks of acceptance, marketing, distribution and use, the Dr Nelson’s Inhaler enjoyed a remarkably speedy rise to fame in the medical marketplace of the 1860s and 1870s. Requiring only steam and cheap non-prescription medication, and readily available from multiple retail outlets – in hospitals and from personal physicians, by mail order catalogue, and from high street chemists or later even drug stores like Boots – the device was one of the most widely used inhalers in the nineteenth century. With its potential to take the treatment of respiratory illness out of hospital wards, physicians’ clinics and spa resorts, the Dr Nelson’s Inhaler offered a reliable form of self-medication against environmentally induced conditions such as bronchitis, catarrh, asthma, and more serious conditions such as the croup or consumption. Similarly, self-medication with the inhaler was connected with prophylactic treatment of respiratory conditions. Rather than allowing one’s health to deteriorate, hence requiring costly treatment by physicians or in hospitals, many of the domestic handbooks and medical treatises point towards personal, preventative treatment in the comfort of the home. Spencer Thomson writes, for example: ‘It is probable that the slow, imperceptible, but continual breathing of an atmosphere impregnated with such medicinal agents […] is more likely to be of service than their temporary use in more powerful doses’ (1866, p 305). Abbotts Smith views inhalation as a form of breathing training, helping to manage the lung function (1866, p 70–71). The emphasis on individual management of respiratory conditions made possible by the Dr Nelson’s Inhaler would later establish itself as a key component in the treatment of asthma patients from the mid-1950s onwards, as new pressurised metered dose inhalers (pMDIs) made self-treatment more reliable and effective (Anderson, 2005, p 1143–1144). Indeed, the instigator behind Riker and Du Pont’s first pMDI in 1956, George Maison, explained that the origins of the project lay in his wish to simplify the treatment of his own asthmatic daughter, finding existing hand-held nebulizer devices unsuitable to outpatient use (see Grossmann, 1994, p 59). While the form of medication may have changed from medicated steam to bronchodilatory powders and steroids (Sanders, 2007, p 79), the ‘cleanliness, portability, and cheapness’ of the Dr Nelson’s Inhaler mentioned in The Lancet (1865a, p 152) are qualities which are still central to inhalation devices today. Indeed, a recent regulatory-industrial collaborative workshop was devoted precisely to developing a patient-use focus in inhalation device design (Roche et al, 2017). Since the mid-twentieth century with Riker’s pMDI and now especially in the twenty-first century, medical device development is returning to Dr Nelson’s maxim of ease and simplicity of use.
Of course, self-medication was by no means unproblematic in the nineteenth century and need not necessarily be considered an indicator of medical or pharmaceutical modernisation. Ineffective and even dangerous household remedies and patent medicines were frequently advertised and consumed in similar ways to the Dr Nelson’s Inhaler, much to the distress and anger of the professional medical classes. A comparison with various other ‘household’ remedies for asthma and consumption in the second half of the nineteenth century confirms this. Alongside more reliable remedies and devices like ‘Vapo-Cresolene’ lamps, pillow inhalers, oxygen bars, asthma cigarettes and pipes (in ascending order of danger), we also find less serious remedies such as ‘Sir Hiram Maxim’s Pipe of Peace’ (Sanders, 2007, p 77), the ‘Carbolic Smoke Ball’, which gained notoriety because of its role in a legal case which defined the limits of promises made in advertisements (Snell, 2001), and even Robert Moffatt’s ‘Ammoniaphone’ (see Dickson, 2017). Given that the Dr Nelson’s Inhaler was accepted in both commercial and professional terms, this was a form of self-medication for in- and outpatients that was medically legitimised. Moreover, it was sanctioned in more formal terms as a treatment method in academic publications such as case histories, medical textbooks, and more widely in domestic handbooks, while the incorporation of steam inhalations in the British Pharmacopoeia in 1867 placed the Dr Nelson’s Inhaler at a remove from these irregular forms of treatment.
Inhalation therapies in the second half of the nineteenth century typically involved either volatile or combustible materials for smoking or vaporisation (Sanders, 2007, p 79), including medicines of herbal origin such as stramonium, a direct link to modern antimuscarinic therapies. However, non-volatile, purified small molecular weight drugs began to emerge from the early twentieth century including adrenaline (extracted from adrenal glands; see Burnett, 1903) in 1903, atropine (purified from Hyoscyamus extracts; see Terray, 1909), ephedrine (structurally-related to adrenaline, purified from Ma Huang herb; see (Chen and Schmid, 1924), and cortisone treatment by the 1950s (see Carryer, 1959). This required an evolution of device technologies to disperse bulk liquids into aerosol droplets that contained the dissolved (or suspended) drug, or to disperse ultra-fine bulk powders of the drug into inhalable aerosols under mechanical or aerodynamic forces. The result of this was the invention and development of the forerunners of modern inhalation devices including jet nebulizers (e.g. the Pneumostat, widely used from the 1930s but still generally housed in surgeries and pharmacies) or hand bulb nebulizers such as the Parke-Davis Glaseptic, and Abbots’ Aerohaler (1948), which is clearly comparable to modern dry powder inhalers, and ultimately the pMDI in the 1950s (Sanders, 2007, p 79).
While steam inhalers were replaced in conventional respiratory medicine by modern inhaler devices, Dr Nelson’s Inhaler is notable for how it helped to establish inhalation as a popular, inexpensive and trusted form of medical therapy for respiratory ailments in the 1860s. In many ways, its inconspicuous ceramic form may well be one reason why it has survived in such numbers to be able to tell this story: unlike later low-cost devices from France and Britain which were made of enamel, the robustness of the Dr Nelson’s Inhaler has helped it to survive in museum collections and antique shops to the present day. As such, the Dr Nelson’s Inhaler can be seen as an important milestone in the development of modern outpatient treatment of asthma and other respiratory conditions. This was not least the case because of its affordability and flexibility, offering simple and reliable relief for respiratory and bronchial patients both in a clinical and a domestic environment. Its emergence from the orbit of the RMCS can also help us to reconstruct a surprisingly thorough framework of what was essentially quality control and professional recommendation, which was highly unusual for pharmaceutical technologies in the nineteenth century. The commercial interests of S. Maw & Son ensured that the inhalation device was widely and successfully marketed and distributed without encroaching on the practices and disrepute of the patent medicine sector of the nineteenth-century medical market. As such the seemingly inconspicuous Dr Nelson’s Inhaler enables us to tell a far-reaching story of pulmonary and respiratory disease and their treatment in the nineteenth century.
Acknowledgements
The research leading to these results was facilitated by the Andrew W Mellon Foundation in the form of a TORCH Knowledge Exchange Fellowship at the Science Museum London.
Tags
Footnotes
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text